by Bethany Blankley
Many individuals considered to be the most at-risk for coronavirus live in states that had the best health infrastructures in place before state restrictions began in March, according to two recent analyses.
Residents of West Virginia, Louisiana, Mississippi, Arkansas, Alabama, Kentucky, Florida, Tennessee, South Carolina and Georgia were found to be the most vulnerable, according to personal-finance website WalletHub’s analysis of States with the Most Vulnerable Populations to Coronavirus.
Whereas states with the best health care infrastructures already in place were North Dakota, West Virginia, Mississippi, Tennessee, Oklahoma, Kentucky, Alaska, Kansas, and Arkansas, according to another WalletHub report.
Individuals with medical vulnerability, housing vulnerability and financial vulnerability living in Arkansas, Kentucky, West Virginia, Mississippi, and Tennessee reside in states with the best health infrastructures in place before the coronavirus shutdown, according to the reports.
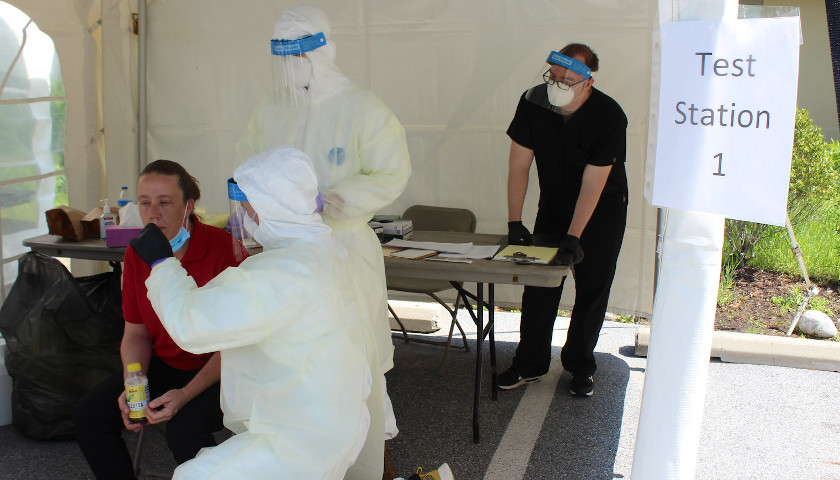
According to data from the Centers for Disease Control, nearly 75 percent of patients hospitalized for the coronavirus are over 50 years old, and 90 percent have pre-existing conditions. The shutdown of state economies and ranges of preparedness highlighted strengths and weaknesses in the U.S. health care system, ranging from the level of supplies, to staffing, to bed counts, WalletHub says.
During the coronavirus shutdown, “the news often focuses on the medically vulnerable – people who risk the most serious symptoms if they contract the disease, such as the elderly or people with pre-existing medical conditions,” WalletHub financial writer Adam McCann said. “However, two other at-risk populations are just as crucial to protect – those who lack adequate living conditions and those without enough monetary resources to weather the pandemic.”
To identify which states have the highest concentration of vulnerable people, WalletHub compared the 50 states and the District of Columbia across 28 key metrics in three overall categories: medical vulnerability, housing vulnerability and financial vulnerability. The data set ranges from the share of the population aged 65 and older to the share of the homeless population that is unsheltered and the share of the entire population living in poverty.
To identify which states have the best health infrastructure, WalletHub compared the 50 states across 14 key metrics. The data set ranges from the state’s Public Health Emergency Preparedness funding per capita to the share of the population that is uninsured and the number of hospital beds per capita.
States with the least vulnerable populations, according to the analysis, are Wisconsin, Wyoming, Connecticut, Iowa, Montana, Vermont, Massachusetts, Minnesota, Colorado and Utah.
States with the worst health care infrastructure are Indiana, New Jersey, Rhode Island, New Hampshire, Arizona, Michigan, New York, Virginia, Maryland and Connecticut.
According to the findings, California has the highest share of the homeless population that is unsheltered (71 percent), about 33 times greater than those living in North Dakota, which has the lowest share of homeless at 2 percent.
Texas has the highest share of the population that is uninsured at 17 percent, which is six times higher than the uninsured rate in Massachusetts, the lowest in the U.S. of 2.8 percent.
North Carolina has the lowest unemployment recipiency rate of 9 percent, which is six times lower than in New Jersey’s, which has the highest in the U.S. of 57 percent.
New York has the lowest Public Health Emergency Preparedness funding per capita of 95 cents.
Vermont has the highest public hospital system quality, whereas New Jersey has the lowest, according to the reports.
Alaska has the highest public healthcare spending per capita of $281 per person, compared to Nevada, which has the lowest spending per capita of $46 per person.
– – –
Bethany Blankley is a contributor to The Center Square.
Photo “Pennslyvania National Guard COVID-19 Tests” by the National Guard. CC BY 2.0.



Are you suggesting that these states with the best health infrastructures with the highest covid rates should get rid of their health infrastructure? As if getting rid of this infrastructure will somehow lower their covid rates?