This is the fifth report in an eight-part series on the Ohio Public Health Advisory System (OPHAS).
OPHAS has seven indicators and each of Ohio’s 88 counties is assigned a color based on the number of indicators that are triggered.
Indicator five measures the sustained increase in outpatient visits for COVID-like illness.
According to the state website, the indicator “provides information on the health care seeking behavior of the population and a sense of how concerned residents are about their current health status and the virus.”
A county triggers this indicator during any five consecutive days over a three week period when there is an increasing trend in the number of people going to a healthcare provider with COVID symptoms (listed below) who then receive a COVID confirmed or suspected diagnosis.
The outpatient data comes from health care providers who assign diagnostic codes to patients, and that information is provided electronically every 24 hours to the Ohio Department of Health (ODH).
ODH Press Secretary Melanie Amato told The Ohio Star that outpatient data for COVID-like illness are provided by “Ohio’s Health Information Exchanges (HIE) as well as one health system (Promedica) that is not part of an HIE.” She continued, “there are two HIEs in Ohio, CliniSync and The Health Collaborative (THC). THC covers the Cincinnati area as well as part of Dayton while CliniSync covers the rest of the state.”
However, the indicator is not COVID-specific. Amato said coding is left up to the doctor who may provide a COVID test or diagnose someone clinically without a test.
“How cases get coded depends on several factors – the availability of tests is one of those factors,” Dr. Elizabeth Laffay, D.O., an emergency and functional medicine physician, told The Star. “When rapid tests are available we can use them at the doctor’s discretion but when they are limited may only use them for patients being transferred to another health care facility, inpatient psychiatric facility or those being admitted to the hospital.”
Laffay added, “The outpatient visits are based on ICD-10 coding and the result of a medical visit is based on how the doctor charts. If a patient or the doctor express COVID concern it could be worded in a way that could end up being coded as a COVID rule out. The physician’s wording in the documentation would trigger a medical coder to code it COVID-like.”
The numbers for COVID-like visits do not equal public health cases as found on the state’s website. “A physician can literally just say it’s COVID and it counts as a clinical diagnosis for the purposes of the health care provider and billing,” said Amato.
To count as an official public health case, a confirmed case must be the result of a positive polymerase chain reaction (PCR) test or clinical diagnosis.
A clinical diagnosis is determined as follows, at least one of the following symptoms:
- fever (measured or subjective)
- chills
- rigors
- myalgia
- headache
- sore throat
- nausea or vomiting
- diarrhea
- fatigue
- congestion or runny nose
OR
Any one of the following symptoms:
- cough
- shortness of breath
- difficulty breathing
- new olfactory disorder
- new taste disorder
OR
Severe respiratory illness with at least one of the following:
- clinical or radiographic evidence of pneumonia
- acute respiratory distress syndrome (ARDS)
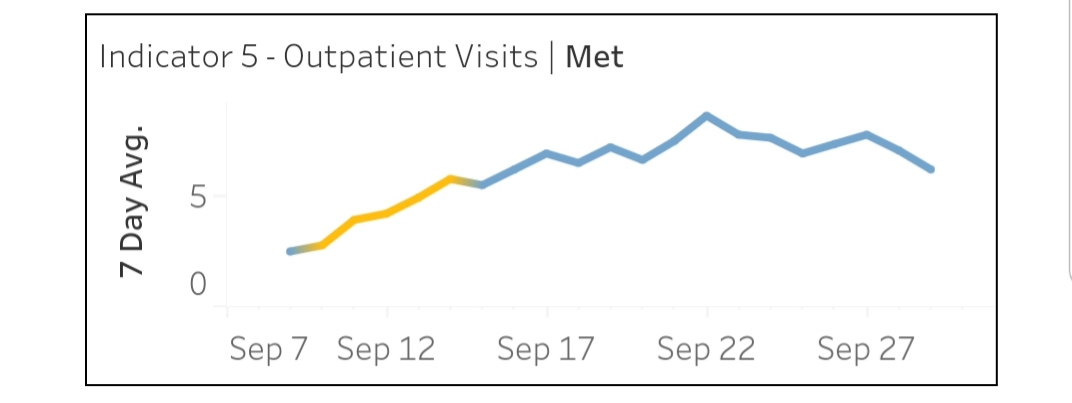
Indicator five has no magnitude control. Ashland County tripped the measure from September 10-14 when the area recorded a small increase in the 7-day average of COVID-like outpatient visits from 2.7 to 5.7.
In the same timeframe, Ashland recorded five COVID-positive cases on September 10 and seven on September 14 – logging zero hospitalizations on both days. Since March, the county has 280 cases, 32 hospitalizations and 5 deaths.
Governor DeWine commented on Ashland County Thursday saying that it remained in red and highlighted the “continued resistance to mask wearing and social distancing in the county.” But the bulk of the cases in Ashland County were recorded at the same time Ashland University brought students back to campus on August 31.
Indicator five is sensitive to symptoms of other illnesses. Outpatient visits for allergies, colds and the flu spike in the fall, according to Live Science. These common ailments have same and similar symptoms as COVID.
According to Laffay, many doctors address COVID in their charting for liability reasons – “to mitigate liability blowback, COVID is often mentioned at some point during charting.”
Therefore as cold and flu season ramp up, indicator five will no doubt be triggered often.
– – –
Jack Windsor is Managing Editor and an Investigative Reporter at The Ohio Star. Windsor is also an Investigative Reporter at WMFD-TV. Follow Jack on Twitter. Email tips to [email protected].
Photo “Coronavirus Patient” by Official U.S. Navy Page. CC BY 2.0.





