by Jamie Keaten and Marilynn Marchione
GENEVA, Switzerland (AP) — A large study led by the World Health Organization suggests that the antiviral drug remdesivir did not help hospitalized COVID-19 patients, in contrast to an earlier study that made the medicine a standard of care in the United States and many other countries.
The results announced Friday do not negate the previous ones, and the WHO study was not as rigorous as the earlier one led by the U.S. National Institutes of Health. But they add to concerns about how much value the pricey drug gives because none of the studies have found it can improve survival.
The drug has not been approved for COVID-19 in the U.S., but it was authorized for emergency use after the previous study found it shortened recovery time by five days on average. It’s approved for use against COVID-19 in the United Kingdom and Europe, and is among the treatments U.S. President Donald Trump received when he was infected earlier this month.
The WHO study involved more than 11,000 patients in 30 countries. About 2,750 were randomly assigned to get remdesivir. The rest got either the malaria drug hydroxychloroquine, the immune-system booster interferon, the antiviral combo lopinavir-ritonavir, or just usual care. The other drugs have largely been ruled out for COVID-19 by previous studies, but not remdesivir.
Death rates after 28 days, the need for breathing machines and time in the hospital were relatively similar for those given remdesivir versus usual care.
The results have not been published in a journal or reviewed by independent scientists, but were posted on a site researchers use to share results quickly.
“The big story is the finding that remdesivir produces no meaningful impact on survival,” Martin Landray, an Oxford University professor who led other coronavirus treatment research, said in a statement.
“This is a drug that has to be given by intravenous infusion for five to 10 days,” and costs about $2,550 per treatment course, he said. “COVID affects millions of people and their families around the world. We need scalable, affordable and equitable treatments.”
Dr. Margaret Harris, a WHO spokeswoman, attributed the difference in the conclusions of the two studies to the fact WHO’s was larger.
“It’s just a much higher-powered study,” she said. “It’s quadruple the number of people in all the other studies.”
However, Dr. Andre Kalil, a University of Nebraska infectious disease specialist who helped lead the U.S. remdesivir study, said the WHO one was poorly designed, which makes its conclusions less reliable. Patients and doctors knew what treatment they were using, there was no placebo infusion to help avoid biased reporting of risks or benefits, there was little information about the severity of patients’ symptoms when treatments began and a lot of missing data, he said.
“Poor quality study design cannot be fixed by a large sample size, no matter how large it is,” Kalil wrote in an email.
Furthermore, the WHO study tested 10 days of remdesivir, so some patients may have been hospitalized longer than they needed to be just to finish treatment, making their length of stay look bad in comparison to others getting usual care.
Remdesivir’s maker, Gilead Sciences, said in a statement that the results are inconsistent with more rigorous studies and have not been fully reviewed or published.
– – –
Jamie Keaten and Marilynn Marchione are reporters for The Associated Press. Marchione reported from Milwaukee.
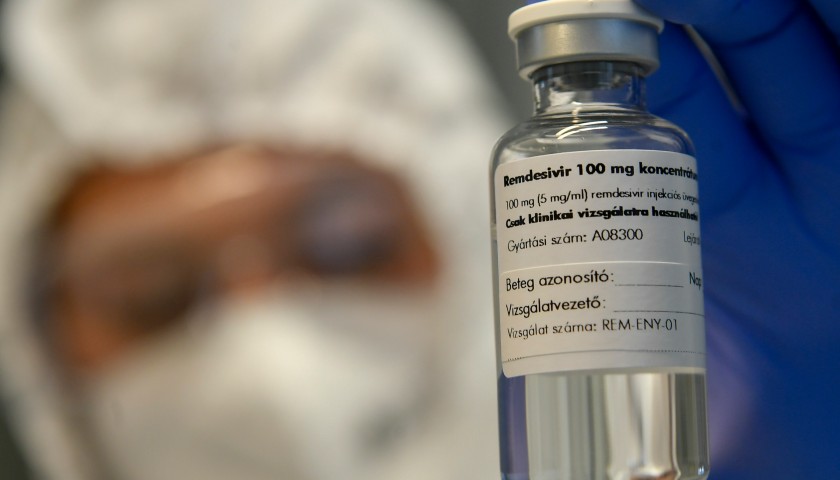
About the Headline Photo: A bottle containing the drug Remdesivir is held by a health worker at the Institute of Infectology of Kenezy Gyula Teaching Hospital of the University of Debrecen in Debrecen, Hungary, Thursday Oct. 15, 2020. A large study led by the World Health Organization released on Friday, Oct. 16, 2020, suggests that the antiviral drug did not help hospitalized COVID-19 patients, in contrast to an earlier study that made the medicine a standard of care in the United States and many other countries. The results do not negate the previous ones, and the WHO study was not as rigorous as the earlier one led by the U.S. National Institutes of Health. But they add to concerns about how much value the pricey drug gives because none of the studies have found it can improve survival. (Zsolt Czegledi/MTI via AP)





Does anyone believe anything that the politicized WHO says? I sure don’t.
There is still a disconnect in the health care industry about how highly effective Hydroxychloroquine, HCQ, is for Covid 19, if it is taken early on when getting the virus. There is a political game going on about it and money is behind it. See the article at: https://theeconomicstandard.com/hcqwhitepaper/ and give the article to your doctor and start asking why they are not prescribing it for people? Frontline doctors treating Covid 19 patients know that it works. I’ve heard directly from a frontline nurse that it works with patients and the patients are making an amazing recovery who use it. There are medical people around the world calling for this thing to be depoliticized and to open up the door for HCQ to be used, with zinc and an antibiotic. Read the Economic Standard report: “Hydroxychloroquine and the Burden of Proof: An Urgent Call to Depoliticize Medicine in the Covid 19 Pandemic.” Granted, we are not in a pandemic anymore; however, let’s get the right treatment available and stop all this fear mongering that is happening.