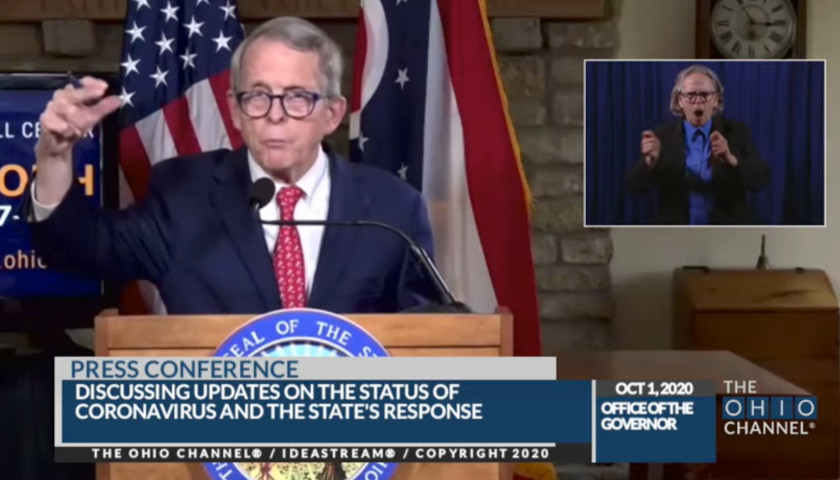
COLUMBUS, Ohio – During the twice-weekly COVID presser, Ohio Governor Mike DeWine invited Dr. Abigail Norris-Turner on Thursday to speak to Ohioans. Norris-Turner revealed the results of a random statewide antibody study former Ohio Department of Health Director Amy Acton mentioned in April and promised May 11.
Regarding the 1,200-person study, Acton said during a press conference on May 11 “[t]hey’re volunteering to help us learn more about the prevalence of this disease, many of whom may not know they have had it.”
Ohio delivered a study involving just over 700 Ohioans. The study was performed in July and sought two findings:
1) People with an active COVID infection;
2) Prevalence of previous infections.
“0.9% of sample had active COVID,” said Norris-Turner, explaining that the number could actually range from between .1% to 2.0%.
The doctor continued by saying “1.5% had evidence of antibodies” to COVID – again explaining that number could be between of 0.3% to 2.9%
According to Norris-Turner, 80,000 Ohioans had COVID during the 20 days in July during which the study was conducted, and 133,000 adults had evidence of past infection.
The U.S. Census data shows Ohio has 11,689,100 people. Based on the number of Ohioans who showed a strong prevalence of antibodies during the July study – using the 1.5% cited – Ohio may have had 175,336 people in July who would have had antibodies across the entire population.
Norris-Turner cautioned about the difficulty of using the numbers from July to make exact assumptions about how many had COVID in previous time periods.
The “assays provide a lookback three months,” meaning the materials used to test the blood samples of Ohioans could find infections only within 90 days.
The doctor went on to say the numbers don’t mean that after three months someone doesn’t have some sort of immunity but “it’s still an open question” as to how much and how strong the immunity.
While answering a question from a reporter on a separate topic, DeWine pointed to the numbers Norris-Turner cited earlier in the presser, saying the numbers are low and indicate the best answer is herd immunity but that we’re “not going to get that without a vaccine” – that we’re going to “work our way into that for years”. Until then we have to “keep this virus low…keep our foot on it’s neck…wait for a vaccine.”
The Ohio Star asked a question of the governor and Norris-Turner to clarify the antibody numbers and state’s direction going forward, handling COVID:
[To Abigail Norris-Turner]: How do you account for people who were infected well before July, because you mentioned that immunity can last three months – or be more easily detected during those three months?
Pike County Department of Health says they had the virus there in November 2019 – a time that would account for close, indoor contact during Thanksgiving, Christmas and New Year celebrations.
We were told that it was more contagious early on.
So there are at least three, 3-month intervals since that time period during which people could have contracted the virus and the immunity could have gone from a strong prevalence easily detectable to having – like you said – some sort of immunity that isn’t detected now.
So, how do you account for people who were infected previously and do those topics get covered in the report?
And governor: Are you now saying that we are in for masking, distancing and quarantining for years?
DeWine kicked off the responses by saying
No. Look, I think the faster the vaccine can get out, the better it is. We have a couple things going for us. And I think this is the reason why people don’t want to get it – and should not want to get it – and that is, doctors have already gotten a lot better at keeping people alive and bringing them back to good health. That will only continue. I think we can expect that to continue. The ability to deal with this once you have COVID will get better, every week. At the same time, the sooner we can get the vaccines out and the sooner people take them – again, been some concern about whether people will take the vaccines – but the sooner we can get to that point, I don’t know what that point is, but that’s what we have to do. That’s what we should do.
But, I can’t put a date on it. There’s no one that I don’t think – any specialist – can put a date on when we will be able to achieve what we need to be able to achieve.
Abigail Norris-Turner said:
What I was saying about that three-month period is just something for everyone to keep in mind. If they get a positive antibody test, they’re screened for COVID – for example they give blood and the Ohio Red Cross tells them that they’re antibody positive, that means that they most likely had infection sometime in the last thee months.
It doesn’t mean that they had it exactly three months ago, it means that they had it sometime in the last three months. Because those are the same assays that we used for this study that was conducted in July, it can only give us a more confident answer related to the number of people that were exposed to coronavirus – not exposed meaning they were at risk of disease – they actually had an infection in the three month period before.
How it relates to earlier in the spring, this study I described today doesn’t tell us about those numbers because the antibody assays don’t capture infections that occurred in that time period. I’ll also say this is just one of the surprises about COVID-19. Folks will know that COVID is cause by SARS-CoV-2 and at fist we were making a lot of inferences about things like antibody levels form our experience with SARs-CoV-1 the virus that cause the original SARS epidemic. For that infection people have antibodies that persist for many months or even years. So the assumption was these antibody tests would give a longer picture, a longer timeline of how many people had been infected. It’s only been in the last few months where there’s more data showing that in fact the timespan is a bit shorter.
To answer your specific question, for example about cases in 2019, I’m not aware of any plausible data that shows that there was circulating virus in Ohio in 2019. And if there were cases in very early 2020 those only were, as folks probably know, only determined after the fact – because of course our first documented infections were on March 9 of this year.
Pike County General Health District reports a case from November 12, 2019.
The Star has reached out to the Ohio Department of Health to find out why the case is not listed in the state’s data file available on the COVID website – and why it’s not considered when making decisions about herd immunity and mitigation policies.
After the press conference, Ohio Lieutenant Governor Jon Husted reached out to The Star through text message -“[i]f I can get you any information about the study let me know. It serves a snapshot for estimates, it does not tell us everything we wish we could know.” The Star requested the full study and the Lt. Governor provided the following link:
What still needs to be determined is the number of Ohioans who had COVID in 2019 and early in 2020, and then determine how many Ohioans have built natural defenses from already having the virus.
A National Institute of Health Study study shows that some people who hadn’t contracted COVID – as high as 57% – already have cells that react as a defense to COVID (SARS-CoV-2) from exposure to other coronaviruses that cause common colds.
The study also notes the T cells may account for the variance of symptoms from COVID – and indicates a significantly larger pool of people who already have COVID defenses.
– – –
Jack Windsor is Managing Editor and an Investigative Reporter at The Ohio Star. Windsor is also an Investigative Reporter at WMFD-TV. Follow Jack on Twitter. Email tips to [email protected].
Photo “Gov. Mike DeWine” by The Ohio Channel.